NIH Awards CSUN Professor $1.45M to Continue Research Targeting Breast Cancer Metastasis
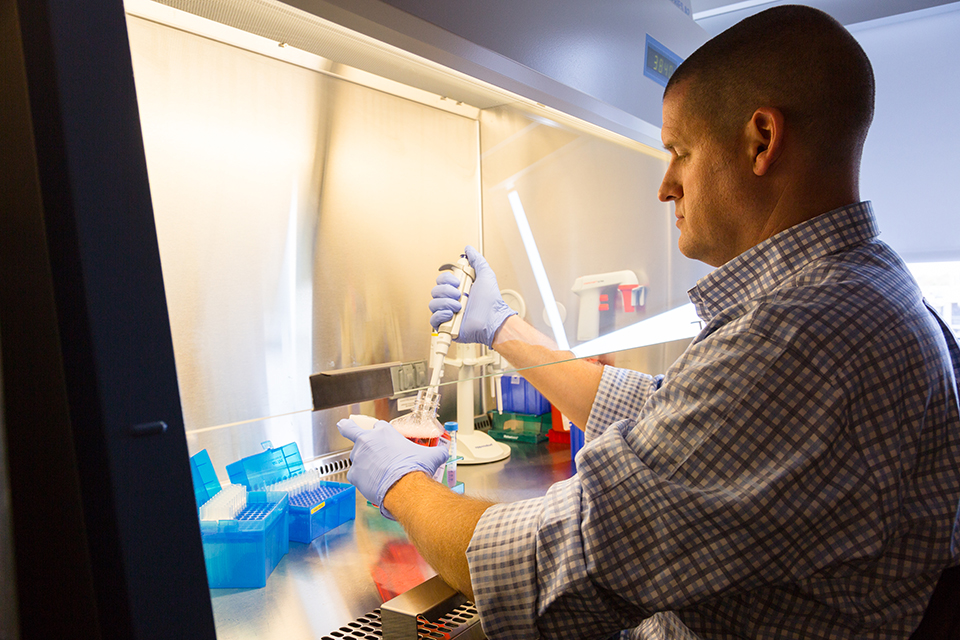
The NIH has renewed a $1.45 million, four-year grant to CSUN biology professor Jonathan Kelber to continue research on breast cancer metastasis. Photo by Allen Birnbach, courtesy of Jonathan Kelber.
The National Institutes of Health (NIH) has renewed a $1.45 million, four-year grant to California State University, Northridge biology professor Jonathan Kelber to continue research on breast cancer metastasis.
Kelber’s research team in CSUN’s Developmental Oncogene Laboratory is searching for new ways to inhibit metastasis — the process of cancer cells moving from their original site of growth to, and growing in, other tissues in the body — in one of the hardest-to-treat forms of breast cancer, triple-negative breast cancer (TNBC).
“Our goal is to understand why and how triple-negative breast cancer cells metastasize,” Kelber said. “Specifically, we are studying how the production of particular proteins influence a cancer cell’s ability to be more aggressive and survive in the foreign tissues to which they spread. This grant will help us take the next steps toward understanding and blocking this process.”
Jonathan Kelber
In 2019, Kelber led his CSUN team of undergraduate, graduate and postdoctoral trainees to identify a small molecule compound that, when delivered to TNBC cells in animal models of metastasis, was able to entirely block this process. Their findings, published in the journal Biochemical and Biophysical Research Communications,described how the molecule GC7 inhibits eIF5A activation and translation of the protein PEAK1 — a critical cancer “support wall” that Kelber’s group was the first to show is essential during the earliest stages of breast cancer metastasis (work published in 2015 in the Public Library of Science (PLoS) One Journal).
In 2017, Kelber received the first four-year cycle of a Research Project Grant (R01)-equivalent, designated SC1 (or Research Advancement Award) from the NIH for his lab to study mechanisms of PEAK1 function in normal and cancerous tissues in breast and pancreas. NIH’s decision to renew this grant, Kelber said, will allow his CSUN team to move beyond the tumor cell-intrinsic mechanisms of metastasis governed by PEAK1 and also study the eIF5A-dependent soluble factors that these metastatic breast cancer cells secrete and pump out to remodel tissues so they are more receptive to the spreading cancer cells.
“These tissues are modified to be supportive of the newly metastasizing cells such that when these traveling cancer cells arrive, the new host tissue unfortunately assists in promoting tumor cell growth and survival,” Kelber said. “In this next cycle of funding, we are specifically looking at how the lung environment is reprogrammed by invasive breast cancer cells in preparation for metastasis. In this context, we have several new molecular interests that we will inhibit and evaluate whether this can render these distant tissues uninhabitable for the cancer cells.
“Ultimately, what we want to do is kill the tumor cells,” he said. “One way of doing that is to prevent premetastatic tissues from becoming fertile soil where these tumor cells can survive. Of course, each tissue to which these cancer cells can metastasize is going to be different. For now, we are focusing on the lung — a common site of breast cancer metastasis.”
This work will be supported by Kelber’s expansive team of collaborators, including Dr. Jack Bui, a professor of pathology at the University of California San Diego School of Medicine, Dr. Julia Tchou, a professor of surgery at the University of Pennsylvania Perelman School of Medicine, and Dr. Isaac Harris, an assistant professor of biomedical genetics at the University of Rochester Medical Center. Notably, to ensure that these studies are clinically relevant, Kelber has secured support from Alana Welm of the University of Utah Huntsman Cancer Institute to employ the institute’s powerful patient-derived xenograft models of breast cancer. These models represent the gold-standard of translational cancer research and ensure that findings in animal models best represent the clinical presentation of the disease. Kelber and his team will learn directly from Welm’s team about how to utilize this valuable resource most accurately as they advance their findings – the goal of which is to help patients.
The NIH recently has approved that principal investigators on SCORE program grants (like Kelber’s SC1) are eligible to apply for diversity supplement awards to support execution of the parent grant.
“We are certainly going to be taking advantage of this program, in an attempt to recruit postdoctoral fellows from diverse backgrounds and to support current undergraduates working on these projects,” Kelber said. “CSUN has expertise and a long history of success in advancing the careers of trainees from backgrounds traditionally underrepresented in biomedical research. I am very excited that my SC1 grant renewal is now eligible for this additional support mechanism from the NIH and I think CSUN will continue to provide an exceptional training environment to advance the training of the next generation of researchers.”

 experience
experience